
Steven, 57, has had hormone therapy. He talks about being diagnosed with stage 4 prostate cancer, how this affected him, and how he now manages his day-to-day life.
Read Steven’s Story in his own words.
“My Prostate Cancer Journey.
In the summer of 2018 I was having issues with passing water, this was low pressure and feeling that I couldn’t empty my bladder, not knowing a lot about prostate cancer, I went to the doctor who sent me for a PSA blood test, when the result came back I was told I was fine, I was not told to keep an eye or return if it persisted.
We now know that whilst a PSA level is a good indicator you really need to have the digital examination, unfortunately this was not done on my visit in 2018, if it had them the rest may have been different.
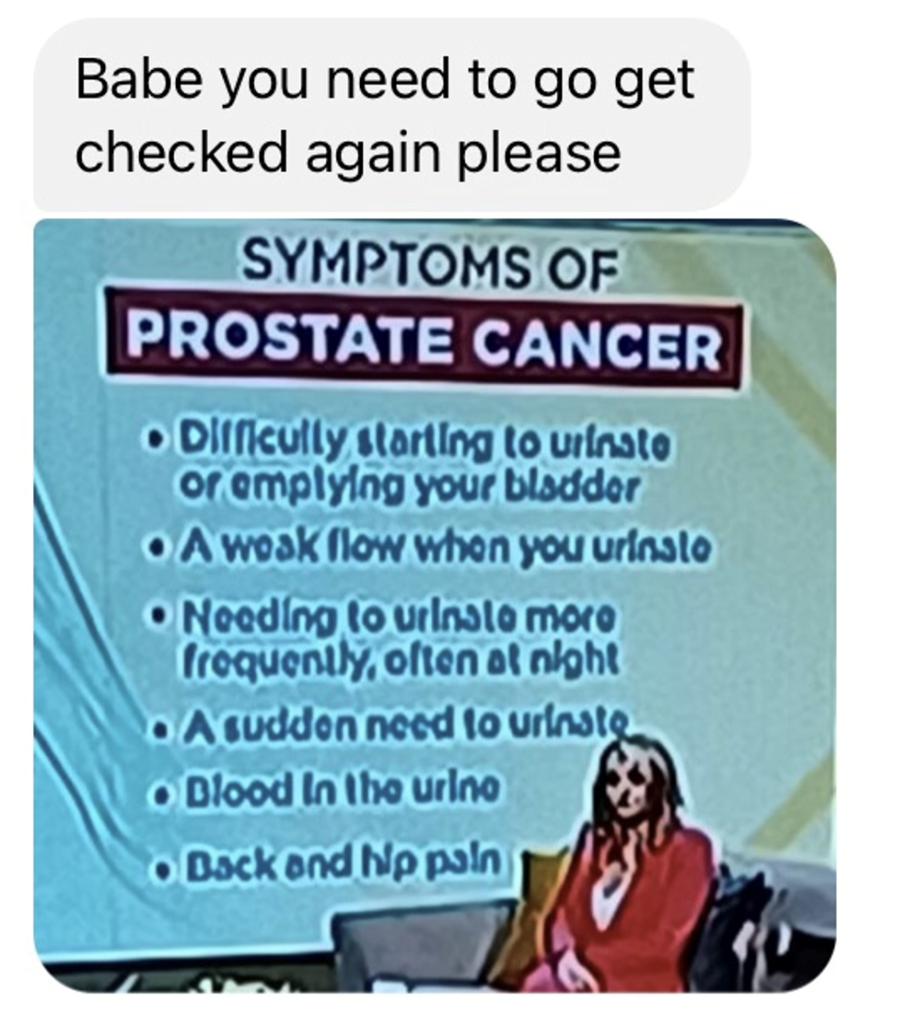
On June 9th 2022 my wife was watching morning TV, the subject that day was prostate cancer, they put up a ‘Symptoms of Prostate Cancer’ on the screen, and my wife instantly recognised that I was showing several symptoms. She photographed the screen and sent me the message shown below. I was showing five out of the six symptoms.
I went to the doctors again that night and had a digital examination. The doctors response to what he felt gave me a good indication that all was not well and I was sent to get a blood test. Two weeks later, the results came back and I was told to wait a further six weeks and then get another blood test. After waiting the six weeks, and then another two weeks, to get the results back, I finally spoke with the doctor and he said that he was now referring me to the urologist, and there was a four week wait time for an appointment. I was now far more up to speed on PSA readings and prostate cancer and asked what my readings had come back at. I was told the first test was ten, and the second test was thirteen. Any PSA level over four should be treated as possible cancer. My reading in 2018 was only two, but from what I know now, I should have had that digital exam and a watching brief should have been employed. To say I was annoyed at the wait is an understatement.
Thankfully, the urologist called me a week later and he sent me information, made an appointment for a MRI scan and a Biopsy to follow, at the Biopsy appointment. We were asked if anyone had spoken to us about the MRI results, and we hadn’t, and it was then that we were told that from the scan, even without the Biopsy, it was definitely cancer, and there was an area in my bowel that was suspicious, the first time you’re told that you never forget, the Biopsy was done and we awaited the results.
About two weeks after the Biopsy we had another pre-arranged call from the Urologist Specialist Nurse. We asked the nurse if we could record the call, and just as well as we did as taking in what we were told was very difficult. We were told that all samples taken contained cancer, with more than half of them showing as an aggressive form, and they gave me a Gleason score of nine and told me that the cancer was incurable but could be controlled for a period of time. The question was asked how long and we were told 50% chance of 5 years. Arrangements were made for my doctor to give me a hormone injection every three months called Prostap 3, and from this point I was referred to the Oncology Department in Singleton Hospital.
Oncology were fantastic, and again over the phone they talked through my situation and booked me in for an isotopic bone scan and a PET scan.
My first face to face meeting with the consultant they discussed the scan results that showed the local lymph nodes were infected and that the area of suspicion was infact cancer. This area was well outside of the prostate lymph nodes, and this put the cancer at Stage 4 Advanced. Treatment options were discussed, and they gave me the options of Chemotherapy or one of the new systemic hormone drugs. After establishing all the ups and downs with both treatments, we opted for the daily hormone drugs. This is a drug called ‘Abiraterone’ taken alongside steroids to counter effect the side effects. Again we asked the question of how long, and were told we should hope for five years.
After three months of Abiraterone I received radiotherapy to two areas, one the prostate and a second area in my bowel. This was completed over 20 sessions and I must say the last two weeks and two weeks after were the hardest time of my life.
So where am I now?
Well, the PSA and testosterone levels are now nondetectable, the hormone drugs do give me massive issues with extreme fatigue, leg pain in my upper legs, hot and cold flushes, and lack of sleep due to flushes, and a side effect from the steroids that induces insomnia. So whilst I try to do my best and live a normal life, it’s not really anything like what I was used to.
I have just passed my six months on the Abiraterone and have just had my first rescans. This has been a CAT scan and Isotope Bone Scan that will show if the cancer has spread into other areasm, and will show how the radiotherapy has affected the cancer.
We have no results yet, so it’s fingers crossed that my results will be back in the middle of June.”
If you have any questions since reading Steven’s Story our Specialist Nurse is a free and confidential service here to help you.
Number: 08000 470 200
Monday – Friday
4pm – 8pm

